What a food and symptom diary is
After stoma surgery, you may be experiencing a number of symptoms you want to change, such as stoma pancaking after your ileostomy or colostomy, or a solution to painful urinary tract infections after your urostomy.
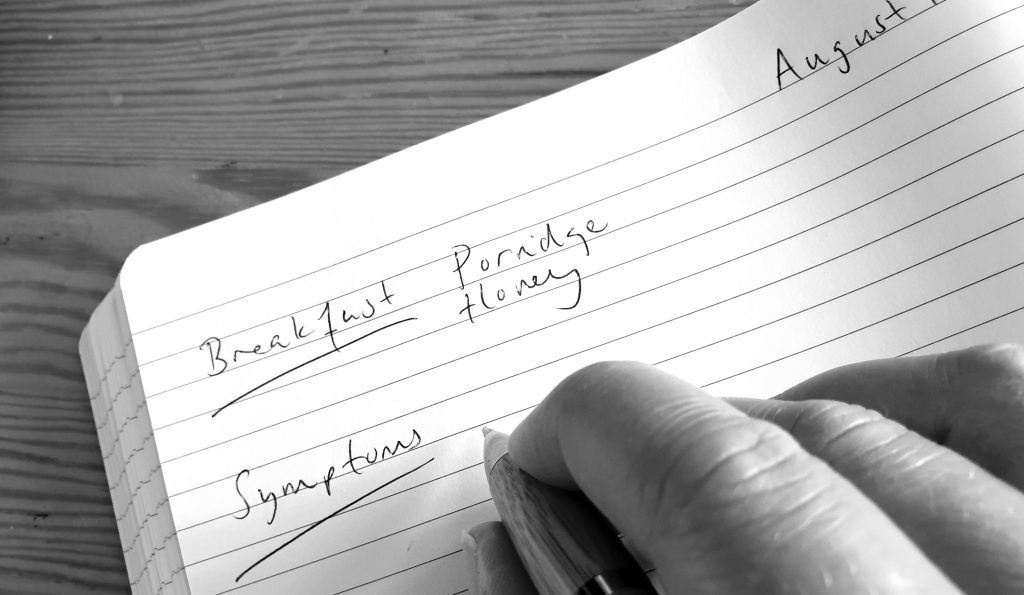
A food and symptom diary is a helpful way to record what you eat and drink that may link to symptoms you’d like to improve. A food diary for ostomates is an important tool.
By keeping a note of the timings of these symptoms, as well as the timings of food, drink, and other useful information e.g. medications, you may be able to see a pattern of triggers which helps identify what changes may be valuable.
It can be helpful to fill in the diary over a few days, both when you have no or mild symptoms, and when your symptoms are worse. This variety can help highlight the differences between these ‘good days’ and ‘bad days’. It’s also helpful to see if symptoms are showing a pattern or are a ‘one off’.
Note: Symptoms can be caused by non-food and drink reasons e.g. stress, missing medications, or medication doses that could be too low or too high. It can be linked to the fit or seal of the pouch against your skin, how regularly your pouch is changed, and what products you use with it. If in doubt, please speak with your medical team.

How to complete your food and symptom diary
For each day of the week, write down what you eat and drink, and the timings. Also write down for that day what symptoms you had and the times they started and stopped. You can also add any notes e.g. if you were stressed, missed any medications, if you did more or less exercise than normal.
How to interpret your completed diary
Step 1)
Notice what symptoms you experience, how often, and if it’s at a particular time of day e.g. very loose stools once a day after breakfast
Step 2)
You can use our handy ‘common stoma problems’ table to see if it matches your symptoms and eating and drinking. If you’d like to, you can try the different steps we’ve suggested for each symptom.
Bowel Stomas & Urostomies Symptoms, Triggers & Solutions
| Problem | Common nutrition triggers | Solutions |
|---|---|---|
| Pouch odour |
Bowel stomasOnions, garlic, broccoli, cauliflower, Brussel sprouts, cabbage, beans, fish, and eggs. UrostomiesDehydration, garlic, asparagus, fish and seafood. |
Step 1If you don’t already, try including dairy foods and parsley that can neutralise unpleasant odours. Step 2Consider some swaps e.g. use asafoetida (hing) powder instead of onion or garlic while cooking, it’s available at most supermarkets. |
| Pouch pancaking |
Bowel stomas
Urostomies – usually non-nutrition related, although may be due to dehydration and passing less urine. |
Sticky stoolsswap fried foods for baked options, choose more tomato-based sauces than creamy options or use less cream. Hard stools and sticky stools – Include foods high in ‘soluble’ fibre e.g. oats, peeled fruit and vegetables, milled seeds. The section of this table on blockages may be helpful. Urostomies, hard stools, and sticky stools – aim for 2L of water a day, with a glass of water with each meal or snack unless you’ve been advised otherwise. |
| Colour changes |
Red:Stools and urine – beetroots, red-coloured berries, red wine and tomato skins Purple/dark blue:Stools – blueberries and blackberries Urine – for those with urostomies, being constipated (not enough water or fibre) Yellow/orange/dark brown:Stools – High fat meals e.g. creamy sauces or fried foods Urine – Very high dose B vitamins or dehydration Green:Stools – High fat meals e.g. creamy sauces or fried foods Black:Stools – Taking iron supplements or bleeding in the digestive system; speak with your Doctor or call the NHS helpline 111 for advice. |
Most colour changes are not harmful and you don’t need to change your diet.
Speak with your Doctor or call the NHS helpline 111 if:
|
Urostomies Symptoms, Triggers & Solutions
| Problem | Common nutrition triggers | Solutions |
|---|---|---|
| Pain when passing urine | Often due to urinary tract infections or urine crystals, which can be caused by:
|
Aim for 2L of water a day, with a glass of water with each meal or snack unless you’ve been advised otherwise.
Choose hydrating foods e.g. fruit and vegetables, soups, and yogurts. You can use our ‘Hydration Guide’ resource. Aim for at least 5 portions of fruits and vegetables a day. At each meal, include 1-2 portions of vegetables, a portion of starchy carbohydrate food, some protein-based food, and around 3 high calcium foods or drinks a day. See our ‘Nutritional Guide’ resource for support. |
Bowel Stomas Symptoms, Triggers & Solutions
| Problem | Common nutrition triggers | Solutions |
|---|---|---|
| Pouch-inflating and bloating | Onions, garlic, broccoli, cauliflower, brussel sprouts, cabbage, beans, chewing gum, fizzy drinks (including beer) and eating quickly. |
Step 1Try chewing your foods very well Step 2Try swapping one of these common triggers at a time, e.g. e.g. green beans instead of broccoli |
| Undigested food and blockages | Minimally chewed food.
Popcorn, bean sprouts, sweetcorn, cooked mushrooms, fruit or vegetable skins e.g. tomatoes, unpeeled cucumber, fibrous food like nuts, seeds, broccoli stalks, celery, and pineapple. |
Step 1Try having smaller portions and chewing these foods very well Step 2If you’ve had multiple reactions to these types of foods, swap them for another e.g. having sharp tasting peeled apples instead of pineapple. |
| Increased stool frequency and watery stools |
|
Step 1Try eating slowly and chewing your food more Step 2Swap to decaf teas and coffees, plain water, water flavoured with fresh fruit slices or ‘cold-infuse’ tea bags Step 3Ensure each meal has a portion of starchy carbohydrates e.g. a fist-sized potato Step 4Try having up to 2 or 3 portions of fruit a day, no fruit juice or smoothies, or up to 150ml a day of fruit juice or smoothies Step 5Swap to foods with more ‘soluble’ fibre e.g. oats, peeled fruits and vegetables, root vegetables. Swap whole nuts or seeds for ground nuts and seeds or nut butter and seed paste e.g. peanut butter and tahini Step 6Try using other strong-tasting herbs and spices instead of lots of chilli e.g. ginger and black pepper Step 7Try drinking water outside of mealtimes e.g. drink in the 15-30 minutes before eating or about an hour afterwards. Still aim for 2L of water across the day unless advised otherwise |
Note: This table was created from a review of reputable information sources and Registered Dietitians’ clinical expertise. This list isn’t exhaustive nor a fool-proof guide to what’s causing your symptoms. It’s always best to seek personalised advice from your personal healthcare professional.
Extra resources:
- Our ‘Nutritional Guide’ and ‘Recipe Booklet’ for advice and suggestions of how to build balanced meals and more information about specific foods and drinks. https://www.fittleworth.com/ostomates-kitchen/
- Our many nutrition and hydration articles written in collaboration with Registered Dietitian Laura Coster https://www.fittleworth.com/blog/
- Our ‘Hydration Guide’ has handy tips for making it easier to drink more and advice on hydrating foods https://www.fittleworth.com/advice-centre/continence/hydration-guidance/
- If you’d like tailored advice, your hospital team can likely refer you to their specialist dietitian. You can also self-refer to a private practice dietitian via the Freelance Dietitians website. https://freelancedietitians.org/
Laura Coster is a Registered Dietitian who is passionate about helping people feel confident in managing their health and find joy through what they eat. 
